Important lessons Covid tests can teach us about STIs

As vaccination programs continue to roll out, many of us in the Western world are starting to feel emboldened enough to return to what we consider “normal.” But, a) the pandemic is not over Againand b) there are extremely important lessons to be learned from the Covid crisis before we go back to the way we did things before. Take the example of STI testing. While the links may not be immediately obvious, the parallels between STI and Covid testing strategies are worth exploring.
Just as the shortcomings of pre-pandemic STI testing may have taught us how to better cope with Covid, the failures of Covid testing can teach us how to pick up the thread and launch an effective STI testing strategy. The Goddess knows that this is absolutely necessary, especially since the realities of Covid-19 have led to a situation where most people facing non-Covid health issues have been left to fend for themselves. Chlamydia and Gonorrhea Testing has fallen by 30 to 50% In spring 2020, staff numbers were down from the previous year as the COVID-19 pandemic stretched the human and staff resources needed, despite a steady increase in STI outbreaks over the past five years, reaching record numbers in 2018. Authorities attribute the increase to rising substandard housing, drug use and social stigma, as well as cuts to sex education and public health budgets.
As COVID-19 rages across the United States, the government has struggled to contain it. Questions about whether to test everyone or just those with symptoms, whether to mandate masks, how best to track infections, and how to effectively engage marginalized communities have come to the forefront. In fact, these and other questions are similar to those that have characterized the fight for effective STI testing for years, as advocates work to reduce infection rates for HIV, syphilis, gonorrhea, and chlamydia, to name a few.
How Covid can help us improve STI screening
While fighting Covid and STIs is a very different experience, the Covid infection cycles are quite similar to the patterns long observed for HIV and TB, where successful suppression of infection is quickly followed by budget cuts (and abandonment of the most deeply affected poor communities of color). The result: infection rates are surging again, what a surprise.
But as a CDC consultant Dr. Hilary Reno “The fact that our resources are being reallocated to fighting COVID-19 makes it particularly important that we now come back and say, ‘If you are sexually active, you should be tested.’”
Here are some key lessons we can learn from the Covid-19 crisis to improve strategies to curb STIs in the future:
1. Shame and fear are ineffective
Julia Marcus, assistant professor at Harvard Medical School, points out that resistance to condom use and resistance to mask use are fueled by some of the same factors misinformation about “manhood.” California Department of Health addresses some of the reasons People resist masks, whether they fear they reflect weakness, fog up their glasses, or have trouble reading facial expressions. Effective STI prevention and mask-wearing campaigns must focus on the protection that wearing a mask provides to both the wearer and the person being worn. And their relatives (in the case of STIs, those very close to them). After all, there have been successes HIV prevention campaigns that appealed to people’s desire to protect not only themselves but also their partners.
2. Promoting abstinence doesn’t work either
Abstinence-only education has Never It worked. Why? Because sexual desire is natural, and any effort to encourage people to ignore or reject it risks backfiring. Former chief public health officer Joycelyn Elders has argued for teaching masturbation in sex education classes as a safer way to explore sex while reducing STIs and unwanted pregnancies, but she got fired for that. Come on America. Just as strict quarantines and social isolation haven’t worked very well (in this part of the world, anyway), making the need for safer, albeit less strict, ways to get through the pandemic ultra-necessary, people need to be educated about safer ways to have sex. Otherwise, people will just believe what’s best for them. If the pandemic has taught us one thing, it’s that strong, clear, concise, and consistent Messaging is an integral part of any popular education initiative.
3. Testing should be free and easily accessible
In the United States, Covid testing has suffered numerous failures, from simple supply shortages to surprise medical billsto almost nonexistent efforts to test people without symptoms. These failures, which have contributed to the spread of the virus, could have been avoided if testing were 100% free, convenient, and accessible to people with and without symptoms. It turns out that most people with STIs are also asymptomatic. The way to get ahead of the curve (remember all that talk early in the pandemic about “flattening the curve”?) is to identify those most at risk and reach them with regular screening and routine testing. In 2014, the CDC recommended that all sexually active women under age 25 be screened annually for chlamydia; this widespread approach has been successful, but STIs like syphilis, without routine testing, have become full-blown epidemics. In the spirit of making testing as convenient as possible, we can draw inspiration from some of the most successful Covid testing initiatives, including mobile van testing for vulnerable neighbourhoods, as well as home test kitsThese are becoming increasingly available and instant home tests are also being developed.
4. Testing should be tailored to disproportionately affected populations
It bears repeating. Like STIs, Covid is much more common among marginalized groups, including communities of color and the poor. Lack of trust in a system that abuses or ignores them creates large segments of the population who would rather forgo testing than participate and engage with the system. Failure to consult marginalized groups in vaccine development results in those who need it most not getting vaccinated. Axios Poll An August 2020 study found that 72% of Black Americans would not get vaccinated, compared to 49% of white Americans. According to Jeanne Marrazzo, a physician and HIV specialist the dish“The only way to get something that works for people is to involve them in the research from the beginning,” she said. “We learned that the hard way in sexual health and we’re making the same mistakes again today.” Moral of the story: Efforts to make STI testing inclusive need to be redoubled. Let’s face it: Meaningful inclusion has always been the only way to go.
In short, the lessons from this experience are a two-way street. Just as we can learn valuable lessons from Covid testing efforts that can be applied to STI testing initiatives, the reverse is also true. If there is one thing that is certain that was not the case before the pandemic, it is that the question “have you been tested/vaccinated?” has joined the ranks of the new gatekeeping questions for lovers; “getting tested” is no longer just about STIs – one could say that our gatekeeping is becoming more holistic, by necessity. Personally, despite my distrust of the system as a whole, I try to remain vigilant about STIs. And I don’t have Covid, so I advocate getting vaccinated and/or getting tested regularly if needed (since you can still catch the virus once vaccinated). You know, all that sexy stuff. <3

 Anal Beads
Anal Beads Anal Vibrators
Anal Vibrators Butt Plugs
Butt Plugs Prostate Massagers
Prostate Massagers
 Alien Dildos
Alien Dildos Realistic Dildos
Realistic Dildos
 Kegel Exercisers & Balls
Kegel Exercisers & Balls Classic Vibrating Eggs
Classic Vibrating Eggs Remote Vibrating Eggs
Remote Vibrating Eggs Vibrating Bullets
Vibrating Bullets
 Bullet Vibrators
Bullet Vibrators Classic Vibrators
Classic Vibrators Clitoral Vibrators
Clitoral Vibrators G-Spot Vibrators
G-Spot Vibrators Massage Wand Vibrators
Massage Wand Vibrators Rabbit Vibrators
Rabbit Vibrators Remote Vibrators
Remote Vibrators
 Pocket Stroker & Pussy Masturbators
Pocket Stroker & Pussy Masturbators Vibrating Masturbators
Vibrating Masturbators
 Cock Rings
Cock Rings Penis Pumps
Penis Pumps
 Wearable Vibrators
Wearable Vibrators Blindfolds, Masks & Gags
Blindfolds, Masks & Gags Bondage Kits
Bondage Kits Bondage Wear & Fetish Clothing
Bondage Wear & Fetish Clothing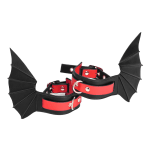 Restraints & Handcuffs
Restraints & Handcuffs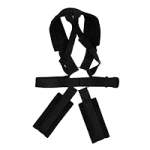 Sex Swings
Sex Swings Ticklers, Paddles & Whips
Ticklers, Paddles & Whips