Vaginismus: Pelvic floor physiotherapy helps women during intercourse

Have you ever experienced unexplained vaginal pain? Even in 2017, there are many vaginal disorders that go untreated, partly due to a lack of education about what these disorders mean. are. One such condition is called vaginismus, or what is now called genitopelvic pain/penetration disorder (GPPD). It is a condition that causes acute tightness in the vagina with no clear immediate cause. We spoke with Amadea Kezar MSc.PTPelvic floor physiotherapist in Montreal, talks about this painful disorder, how it manifests itself and the steps to take to treat this condition.
As with many health issues, it is essential to be aware of the pain and reduce the anxiety associated with the discussion. “Although women may acknowledge that their vagina feels ‘tight’ or ‘blocked’ during sex, that it is impossible to insert a tampon, or that their knees involuntarily close at the gynecologist, they often do not say anything… They think they are the only ones who feel this way. [this pain]because in the media, sex is presented as something easy and pleasant.
This perception makes women shy about why they seek medical attention, and doctors do not regularly seek out new cases.
Kezar’s office sees three to four cases a month, but she says the safety of her office allows people to be more open about discussing symptoms:[Our patients] “Women know they are seeing a health professional they have been referred to. For others, who feel ‘abnormal’, ‘embarrassed’ and ‘ashamed’, it is more difficult.” In some clinics, these vague notions of pelvic pain or discomfort are brushed aside by health care providers. “In our clinic, we encourage all patients to become pelvic health ambassadors and start talking about their experiences and treatment procedures with their friends so that other women will come forward. Once the taboo is broken, women will be able to access services more quickly.”
It is often unclear which came first: the GPPD or the anxiety.
While it is important to be open to this disorder, it is important to seek professional help to properly identify this condition. Medical literature agrees that vaginismus or GPPD, although manifesting itself in a very physical way, is in many cases an anxiety-based disorder. Kezar offers some tips to help women identify it themselves.
She notes:
“In most cases it is impossible to identify an exact cause [of Vaginisimus]Patients will acknowledge that they experience anxiety or fear specifically related to vaginal intercourse, but they are often unsure what the initial triggers may have been. It is often unclear which came first, the bipolar disorder or the anxiety. It is important to know that you do not have to be a generally anxious person to experience vaginismus. Triggers can be physical, emotional, or a combination of both, and it may take some research to identify the culprit. Examples include a previous vaginal or urinary tract infection, lack of adequate lubrication during intercourse, a tender scar from vaginal delivery, or a rough speculum exam. Emotional triggers can be anything that causes stress. Research shows that women who are under stress from a perceived threat actually contract their pelvic floor in a protective manner!1 Whatever the trigger, the pelvic floor muscles contract protectively, like you’re removing your hand from a hot stove. This reaction can cause pain, and then every time you try to insert something into the vagina, you anticipate the pain, which is enough to trigger the contraction, which can become an uncontrollable cycle.
Demystifying the vagina is essential
There is hope, though. Kezar’s clinic is one of many that can help women feel better about the condition and ease their pain. It’s important to note that whether you self-diagnose or are diagnosed by a doctor, “you don’t need a referral to see a pelvic health physiotherapist. So we really encourage women to come talk to us. Even if a woman isn’t sure if she has GPPD, come and ask her what she’s going through. We all have a network of medical and mental health professionals who can help you. We’ll mobilize our resources to find a solution.”
If you’re one of the many women who struggle with discomfort, Kezar and her team offer comprehensive pelvic floor physical therapy. In order to alleviate a condition that has both physical and mental causes, Kezar’s team offers a holistic approach to help treat it: “It all starts with inviting the patient into a safe space where we can have an open conversation about what she’s been through and what her goals are.” Women participate in guided body education conversations in hopes of breaking down protective feelings that may be causing the tension. “Slowly, women will be guided through relaxation and body discovery exercises. Some women have never seen “They have discovered their vulva, let alone explored it. It is essential to demystify the vagina and break down misconceptions about sexual intercourse.”
“There is no pressure to perform an internal exam or even undress, and initially we can focus entirely on breathing exercises. We never want our approach to be perceived as threatening, and we have a toolbox of strategies to help women dismantle their protective responses to comfortably allow vulvar contact and eventually vaginal insertion.”
Partners should be involved in treatment
Once the dialogue is open with the patient, Kezar and her team begin the physical therapy process. “We will gradually introduce exercises that challenge her responses to touch: a beginner technique is to have our patient accept light pressure on the leg that progresses towards the vulva, then the gradual insertion of a finger or a small dilator into the vagina, which will eventually enlarge. Partners are encouraged to participate in the process. When the patient feels comfortable and confident, she can re-explore sexual intercourse, which can happen after about 6 to 12 sessions.”
The dilators Kezar uses in pelvic floor physiotherapy are popular in treating vaginismus, but should be used under supervision: “I see too many patients who have already been told by another healthcare professional to just ‘start working with dilators.’ In my opinion, that’s unacceptable. You wouldn’t tell someone who’s afraid of spiders to just go and handle them, so I don’t understand why that mentality applies to something much more intimate. It’s not a do-it-yourself thing – women need guidance.”
When used effectively, dilators deliver real results: “Treatment works best when women are guided and encouraged through a step-by-step program that builds their confidence and control over their bodies. Specifically, patients must learn to find and control the relaxation of their pelvic floor muscles so that they can allow for comfortable insertion.”
Like many other disorders and stresses, vaginismus is a treatable condition that will become less of an individual stressor as our gender shares more of its findings, advice, and remedies. Kezar and her team are just one of the clinics that can help ease this pain, and their services are highly recommended: “Having a trained pelvic health physical therapist help them through the process and demystify what the patient is experiencing can save them a lot of time and, frankly, trauma. We understand the courage and vulnerability involved in seeking help and going through the process. We train so that we can help women through this time and give them hope that there is a solution… come ask.”
Stay up to date on all things pelvic health by following Amadea Kezar on Instagram and Facebook!
Academic source: Van der Velde, J. and Everaerd W. (2001), The relationship between involuntary pelvic floor muscle activity, muscle awareness, and perceived threat in women with and without vaginismus, Int Urogynecol J, Pelvic floor dysfunction, 12328-31

 Anal Beads
Anal Beads Anal Vibrators
Anal Vibrators Butt Plugs
Butt Plugs Prostate Massagers
Prostate Massagers
 Alien Dildos
Alien Dildos Realistic Dildos
Realistic Dildos
 Kegel Exercisers & Balls
Kegel Exercisers & Balls Classic Vibrating Eggs
Classic Vibrating Eggs Remote Vibrating Eggs
Remote Vibrating Eggs Vibrating Bullets
Vibrating Bullets
 Bullet Vibrators
Bullet Vibrators Classic Vibrators
Classic Vibrators Clitoral Vibrators
Clitoral Vibrators G-Spot Vibrators
G-Spot Vibrators Massage Wand Vibrators
Massage Wand Vibrators Rabbit Vibrators
Rabbit Vibrators Remote Vibrators
Remote Vibrators
 Pocket Stroker & Pussy Masturbators
Pocket Stroker & Pussy Masturbators Vibrating Masturbators
Vibrating Masturbators
 Cock Rings
Cock Rings Penis Pumps
Penis Pumps
 Wearable Vibrators
Wearable Vibrators Blindfolds, Masks & Gags
Blindfolds, Masks & Gags Bondage Kits
Bondage Kits Bondage Wear & Fetish Clothing
Bondage Wear & Fetish Clothing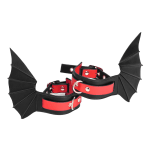 Restraints & Handcuffs
Restraints & Handcuffs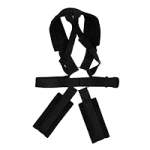 Sex Swings
Sex Swings Ticklers, Paddles & Whips
Ticklers, Paddles & Whips