The Post-Chemo Guide to Sex | Aldult Toys Blog

Fact: In one way or another, cancer and its treatments will change your body. And it’s entirely possible that your sense of sexuality and your sex life will be part of those changes.
Let’s face it, cancer can have a negative impact on sexuality, both physically and emotionally. Most people diagnosed have very legitimate concerns about their sex lives.Before, duringand after chemotherapy treatments.
But here’s the thing: a) this too shall pass, and b) sex is a world unto itself with countless expressions of sensuality, excitement, and release.
Managing sexuality after cancer
How you do after chemotherapy will depend largely on the specifics of your case: how you feel, what type of cancer you have, what stage it is, and what type of chemotherapy you received. Just to name a few.
After chemotherapy, some people choose to wait a while before having sex. Others, on the contrary, are eager to get started. Some stop their sexual activity as soon as they are diagnosed, others during treatment, while still others never stop having sex.
Whatever the details of your experience so far, it’s good to know that sometimes new sexual problems appear shortly after treatment, and some even develop months or years later. That said, and I understand you, take a breath instead of panicking, because if you want this, you’ll get it.
When Your Sex Life Is Compromised After Chemo
After chemotherapy, it’s very common to struggle with the emotional side of sex: body image issues are common, especially if you’ve lost a breast or are dealing with decreased fertility, for example, but also more generally. A decreased libido and a decreased desire for intimacy are also quite common. Some people experience negative thoughts and feelings during sex and/or have trouble feeling sexual arousal, pleasure, or orgasm. All of this is understandable given the circumstances. It is just the way it is. Suffice it to say, though, that if you’re in a relationship, it can be challenging in an entirely different way. Couples therapy, however, has helped many consenting couples recover and reconnect after cancer.
Many women also face physical obstacles. Penetrative sex may have become painful at one point or another. Some experience genital pain when touched. Vaginal dryness and tightness can also become a problem. Add to this the fact that half of breast cancer survivors and other cancers that affect the pelvic area (including the cervix, ovaries, uterus, bladder, colon, and vagina) develop long-term sexual problems. Most of these problems are actually caused by treatment and not the cancer itself. Chemotherapy can also damage the ovaries and trigger hormonal changes, infertility, and menopause (temporary or permanent) in younger women.
Yeah, that’s a lot.
But again, here’s the thing: a) this too shall pass, and b) sex is a world unto itself with countless expressions of sensuality, excitement, and release.
The good news: you are strong, you are alive, and you are equipped to cope.
In Search of Sexual Healing
If you are experiencing emotional and/or physical barriers to sexuality, sex, or intimacy, consider taking the following steps:
Check your medications. Ask a member of your healthcare team to check if your medications could cause side effects, whether physical or emotional (for example, difficulty reaching orgasm or depression). Sometimes, changing your medication, changing the dose, or developing a plan to wean yourself off of them is all it takes.
Consult a licensed mental health professional. Never underestimate the ability of a qualified therapist (for yourself and/or your partner) to help you overcome a loss of sexual desire or intimacy. Your feelings may be related to depression, anxiety, low self-esteem, or relationship conflict. Or all of these. After all, you have just undergone cancer treatment.
Consult a pelvic floor specialist. Talk to an experienced pelvic floor therapist who has experience with painful intercourse and cancer survivors. They will likely teach you that the nerves that allow you to feel pleasure around your clitoris and vagina are very rarely damaged by chemotherapy. They can also teach you invaluable things: relaxation and offering methods dilator exercises that strengthen the vaginal muscles, both of which help overcome pain.
Consult a gynecologist or endocrinologist. Educate yourself about the symptoms of early menopause you may be experiencing, as well as any vaginal dryness or tightness, and get your hormone levels checked promptly. Also seek advice on using over-the-counter vaginal moisturizers for sexual activity. You can also look into low-dose vaginal estrogen in cream, tablet or ring form – some women find these products life-changing.
Explore alternatives for starting a family. Because every person is different, it’s difficult to predict how chemotherapy will impact fertility. The outcome often depends on the type and stage of cancer, medications and dosages, radiation therapy, surgeries, age, and genetics. Ultimately, it’s important to know that people who have undergone treatment are at a higher risk of infertility and birth defects. If you’re planning on having children in the future, talk to your doctor about ways to preserve your fertility. This could include freezing sperm, eggs, or even embryos. Other options include sperm, egg, or embryo donation, surrogacy, and adoption.
Communicate with your partner. If you’re having trouble feeling pleasure or arousal during sex, or if you’ve lost feeling in an area of your body that used to give you a lot of pleasure, communicate with your partner. Together, you can find new types of touch that you enjoy. For example, certain positions can help prevent pain during sex. Even if this has been the biggest challenge, it could ultimately strengthen your bond. A lot.
Consult a sexologist. If communicating with your partner doesn’t work, ask for a referral to a qualified couples sexologist who specializes in treating cancer survivors.
Discover herbal remedies. If you have an herbal remedy you would like to try, talk to your healthcare professional first to avoid any negative interactions with other medications you may be taking.
Bottom line: You may be used to thinking of sex as just intercourse. But sex can be any type of intimate touch or act that makes you and your partner feel good and connected. Your sex life will likely be different after chemotherapy, but with time and effort, you can have a fulfilling sex life again—and maybe even better than before. <3

 Anal Beads
Anal Beads Anal Vibrators
Anal Vibrators Butt Plugs
Butt Plugs Prostate Massagers
Prostate Massagers
 Alien Dildos
Alien Dildos Realistic Dildos
Realistic Dildos
 Kegel Exercisers & Balls
Kegel Exercisers & Balls Classic Vibrating Eggs
Classic Vibrating Eggs Remote Vibrating Eggs
Remote Vibrating Eggs Vibrating Bullets
Vibrating Bullets
 Bullet Vibrators
Bullet Vibrators Classic Vibrators
Classic Vibrators Clitoral Vibrators
Clitoral Vibrators G-Spot Vibrators
G-Spot Vibrators Massage Wand Vibrators
Massage Wand Vibrators Rabbit Vibrators
Rabbit Vibrators Remote Vibrators
Remote Vibrators
 Pocket Stroker & Pussy Masturbators
Pocket Stroker & Pussy Masturbators Vibrating Masturbators
Vibrating Masturbators
 Cock Rings
Cock Rings Penis Pumps
Penis Pumps
 Wearable Vibrators
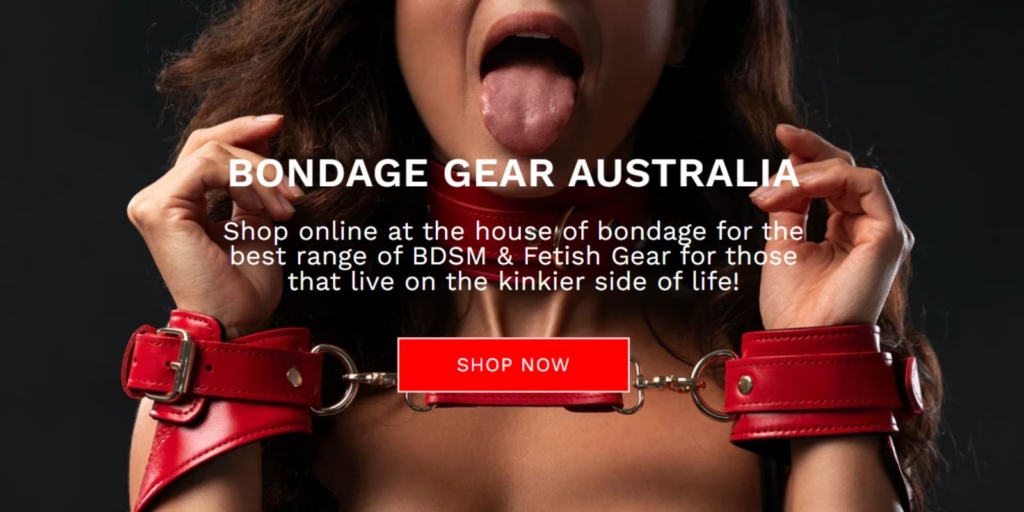
Wearable Vibrators Blindfolds, Masks & Gags
Blindfolds, Masks & Gags Bondage Kits
Bondage Kits Bondage Wear & Fetish Clothing
Bondage Wear & Fetish Clothing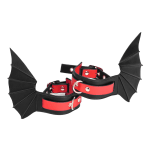 Restraints & Handcuffs
Restraints & Handcuffs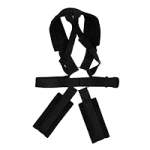 Sex Swings
Sex Swings Ticklers, Paddles & Whips
Ticklers, Paddles & Whips